Facts
Chronic obstructive pulmonary disease (COPD) is a long-term lung disease that makes it hard to breathe.
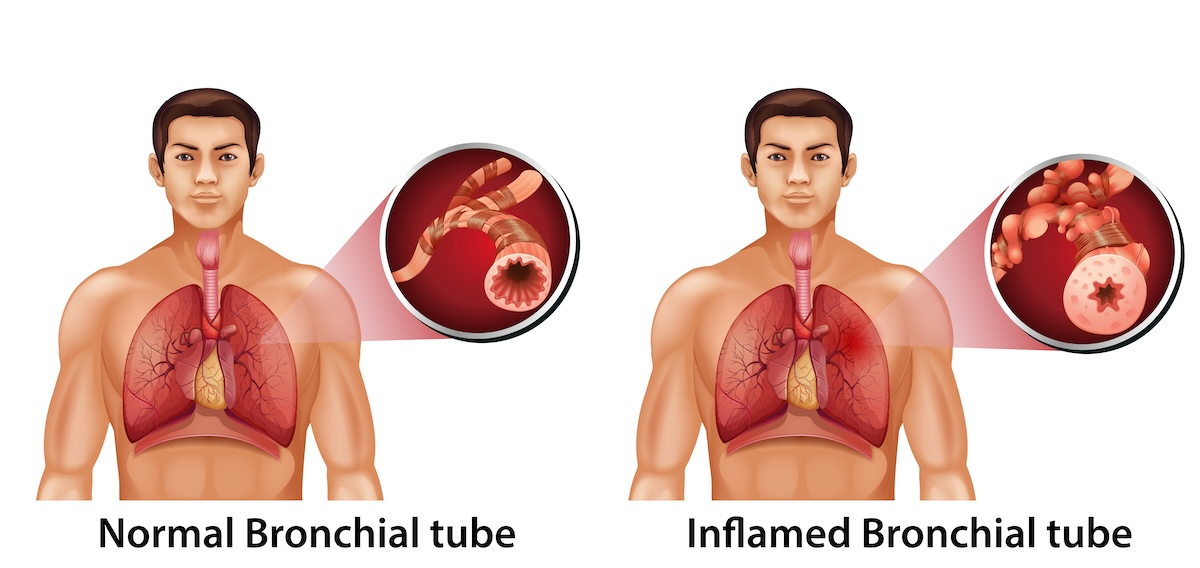
It happens when the airways (the tubes that carry air in and out of your lungs) become inflamed and narrowed and the air sacs (alveoli) in the lungs are damaged. This limits airflow in and out of the lungs. The damage is usually permanent and gets worse over time, progressively getting worse.
COPD is caused by two conditions:
- Chronic bronchitis: long-term inflammation of the airways that causes cough and mucus.
- Emphysema: damage to the air sacs, making it hard for the lungs to take in oxygen.
People with COPD often feel short of breath doing everyday activities because their lungs can’t move air in and out as easily as in people with healthy lungs.
According to the Lung Foundation of Australia, around 1 in 13 people over 40 have COPD. Over 50% of those people have not been diagnosed with this condition, so they are not aware they have this disease. Indigenous Australians have a higher risk of developing this disease (2.2x more) than non-Indigenous Australians)
Symptoms
Chronic obstructive pulmonary disease symptoms
Early diagnosis and treatment can slow COPD progression. If you experience persistent cough, shortness of breath or increased mucous production, especially if you have risk factors like smoking history, consult a healthcare provider for proper evaluation and lung function testing.
Early stage symptoms
In the early stages of COPD, symptoms are often subtle and may be mistaken for a cold, sinusitis, hay fever, mild respiratory infection, normal signs of aging or being out of shape:
Mild shortness of breath
- Initially occurs only during physical exertion like climbing stairs or brisk walking
- May be dismissed as lack of fitness
- Gradually becomes more noticeable with less strenuous activities
Chronic cough
- Often called “smoker’s cough” by those who smoke
- May be dismissed as normal, especially by smokers
- Can be dry or productive (producing mucus)
- Often worse in the mornings or at night
Mild mucous production
- Clear or white phlegm
- More noticeable in the morning
- May increase during respiratory infections
Occasional wheezing
- Mild whistling or squeaky sound when breathing
- More noticeable during exertion or when lying down
Moderate stage symptoms
As COPD progresses and gets worse, symptoms become more persistent and can interfere with daily activities:
Increased shortness of breath
- Occurs with everyday activities like walking on flat ground, getting dressed, or showering
- May need to stop and rest frequently during activities
- Breathing becomes noticeably more difficult
Persistent cough
- Becomes more frequent and bothersome
- May occur throughout the day and night
- Can disrupt sleep
Increased mucous production
- Greater volume of phlegm
- May be thicker and harder to expel
- The colour may change to yellow or green during infections
Frequent wheezing
- More constant and louder, very audible to everyone
- May be heard even at rest
- Can be accompanied by chest tightness
Reduced exercise tolerance
- Difficulty completing previously manageable tasks
- Require more frequent rest periods
- Avoidance of physical activities
Fatigue
- Persistent tiredness unrelated to activity level
- Due to extra effort required for breathing
- Can affect quality of life significantly
Severe and late stage symptoms
In advanced COPD, symptoms are severe and significantly impact quality of life:
Severe shortness of breath
- Occurs even at rest or with minimal activity
- Difficulty breathing while eating, talking or performing basic self-care
- May need to sleep in a semi-upright position
- Can cause anxiety and panic
Chronic respiratory infections
- Frequent bronchitis infections and possibly pneumonia
- Longer recovery times
- Exacerbations (flare-ups) may require hospitalisation
Cyanosis
- Bluish discoloration of lips, fingernails, or skin
- Indicates insufficient oxygen in the blood
- Medical emergency requiring immediate attention
Unintended weight loss
- Due to increased energy expenditure from breathing effort
- Loss of appetite from fatigue and shortness of breath
- Muscle wasting (cachexia)
Swelling in ankles, feet or legs (peripheral oedema)
- Caused by heart complications (cor pulmonale)
- Results from strain on the right side of the heart due to lung disease
- May indicate right-sided heart failure
Barrel chest
- Chest appears rounded and enlarged
- Due to air trapping in the lungs
- Ribs appear more horizontal
Use of accessory muscles
- Visible use of neck and shoulder muscles to breathe
- Pursed-lip breathing (breathing out through pursed lips)
- Nostrils flaring with each breath
Confusion or memory problems
- Due to chronic low oxygen levels (hypoxemia)
- Can affect concentration and mental clarity
- May worsen during exacerbations
Morning headaches
- Caused by carbon dioxide buildup during sleep
- Can indicate respiratory failure
Decreased oxygen saturation
- May require supplemental oxygen therapy
- Finger oxygen monitors show levels consistently well below 90%, whereas healthy oxygen levels should be between 95%-100%
Causes
Causes of chronic obstructive pulmonary disease
Primary causes
These are the main causes of COPD
Cigarette smoking (leading cause)
- Responsible for 85-90% of all COPD cases
- The most significant risk factor worldwide
- Both active smoking and long-term exposure to second hand smoke cause damage
- Risk increases with:
- Number of cigarettes smoked per day
- Duration of smoking (pack-years)
- Age when smoking started
- Even former smokers remain at elevated risk
- Pipe, cigar and marijuana smoking also contribute
Secondhand smoke (passive smoking)
- Exposure to others people’s cigarette or cigar smoke
- Particularly dangerous for children and non-smoking adults
- Long-term exposure in homes or workplaces increases risk
- Can contribute to COPD development even without personal smoking history
Occupational exposures
- Prolonged exposure to workplace dusts, chemicals, and fumes
- High-risk occupations include:
- Coal mining
- Construction work
- Metal work and welding
- Grain and flour processing
- Textile manufacturing
- Chemical manufacturing
- Agriculture (exposure to organic dusts)
- Industrial pollutants like:
- Silica dust
- Cadmium dust
- Coal dust
- Asbestos
- Chemical vapours and fumes
Air pollution
- Outdoor air pollution from vehicle emissions and industrial sources
- Indoor air pollution, particularly in developing countries:
- Burning wood, coal, or biomass fuels for cooking and heating
- Poor ventilation in homes
- Cooking smoke exposure affects millions globally, especially women
Genetic factors
- Alpha-1 antitrypsin deficiency (AAT deficiency):
- Some people are born with a deficiency of a protective protein called alpha-1 antitrypsin.
- It’s a rare genetic disorder (1-2% of COPD cases)
- It’s an inherited lack of the AAT protective protein in the lungs
- Can cause COPD even without smoking
- Leads to early-onset COPD (age 30-40)
- More severe in smokers with this deficiency
- Other genetic variations may increase susceptibility to smoking damage
Contributing factors and risk factors
Childhood respiratory infections
- Severe respiratory infections during childhood
- Can impair lung development
- May increase susceptibility to COPD later in life
Asthma and airway hyper-responsiveness
- Long-standing asthma increases COPD risk
- Chronic airway inflammation can lead to permanent changes
- Asthma-COPD overlap syndrome (ACOS) is increasingly recognised
Age
- COPD typically develops after age 40
- Risk increases with age due to cumulative exposure
- Lung function naturally declines with aging
Socioeconomic status
- Lower socioeconomic groups have higher rates
- May be related to:
- Higher smoking rates
- Increased occupational exposures
- Poor indoor air quality
- Limited access to healthcare
- Nutritional deficiencies
Poor nutrition
- Malnutrition or vitamin deficiencies may affect lung health
- Low antioxidant intake may reduce lung protection
- Underweight individuals may have increased risk
How COPD develops and damages the lungs (pathophysiology)
Chronic inflammation
- Irritants trigger inflammatory response in airways
- White blood cells release enzymes that damage lung tissue
- Inflammation becomes chronic and persists even after exposure stops
Emphysema
Emphysema causes:
- Destruction of alveoli (air sacs) walls
- Loss of elastic recoil in lungs
- Air becomes trapped, causing hyperinflation
- Reduces surface area for oxygen exchange
Chronic bronchitis
Chronic bronchitis causes:
- Inflammation and thickening of bronchial tubes
- Excess mucus production
- Damaged cilia (tiny hairs that clear mucus)
- Narrowed airways obstruct airflow
Small airway disease
- Narrowing and scarring of small airways
- Contributes significantly to airflow limitation
- Often occurs early in disease process
Risk factors
Highest risk
- Current heavy smokers (1+ pack/day for 20+ years)
- People with Alpha-1 antitrypsin deficiency who smoke, this protein is a cause of emphysema in a small percentage of people
- Workers with long-term occupational dust or fume exposure who also smoke
Moderate risk
- Former smokers with significant smoking history
- Long-term secondhand smoke exposure
- Occupational exposures without smoking
- Indoor biomass fuel exposure
Lower but notable risk
- People with childhood respiratory problems
- Those with chronic asthma
- Genetic predisposition in family history
Prevention
Understanding causes helps with prevention:
- Never smoke or quit smoking (most important)
- Avoid secondhand smoke
- Use proper protective equipment in hazardous work environments
- Improve indoor air quality
- Use cleaner cooking fuels like electricity
- Reduce exposure to outdoor air pollution when possible
- Get vaccinated against respiratory infections
- Genetic testing for those with family history of early COPD
Prevention
Prevention of chronic obstructive pulmonary disease
Most COPD cases are preventable. The single most effective way to prevent COPD is to never start smoking or to quit if you currently smoke. Even in people with genetic predisposition, avoiding smoking and avoiding other risk factors can dramatically reduce the likelihood of developing the disease.
If you have risk factors for COPD, especially a smoking history, talk to your healthcare provider about lung function testing (spirometry) to detect the disease early when interventions are most effective.
- Don’t smoke — quitting at any stage helps slow lung damage.
- Avoid second-hand smoke and polluted air.
- Use protective masks if you work around dust, fumes, or chemicals.
- Stay active and maintain a healthy weight.
- Get vaccinated for flu and pneumonia to prevent infections that worsen COPD
Complications
Complications of chronic obstructive pulmonary disease
If COPD isn’t managed well, it can lead to the following very severe complications:
Pulmonary hypertension
- High blood pressure in lung arteries
- Strains the right side of the heart
Depression and anxiety
- Common due to lifestyle limitations
- Fear of breathlessness can cause panic attacks
- Social isolation from inability to participate in activities
3. Sleep Disturbances
- Difficulty sleeping due to breathing problems
- May have sleep apnea
- Frequent nighttime awakenings
Acute Exacerbations
At any stage, COPD patients can experience exacerbations (flare-ups) with worsening symptoms:
- Sudden worsening of shortness of breath
- Increased cough and mucus production
- Change in mucus colour (yellow, green or brown)
- Increased wheezing
- Chest tightness
- Fever
- Confusion or drowsiness
Diagnosis
Chronic obstructive pulmonary disease diagnosis
COPD is diagnosed through the following assessments. Your doctor will decide which tests they will do after the initial assessment:
Initial assessment
Medical history – Your doctor will begin with a detailed medical history, asking about:
- Smoking history: Current and past tobacco use (pack-years calculation)
- Occupational exposures: Work history involving dusts, chemicals, or fumes
- Environmental exposures: Indoor/outdoor air pollution, secondhand smoke
- Symptom details: When symptoms started, severity, frequency
- Family history: COPD or Alpha-1 antitrypsin deficiency in relatives
- Previous respiratory infections: Childhood illnesses, recurrent bronchitis
- Other medical conditions: Asthma, allergies, heart disease
- Current medications: Including over-the-counter drugs
- Limitations: Impact on daily activities and quality of life
Physical examination – The doctor will perform a thorough physical exam:
- Listening to lungs: Using a stethoscope to detect wheezing, decreased breath sounds, or crackles
- Breathing pattern observation: Looking for use of accessory muscles, pursed-lip breathing
- Chest examination: Checking for barrel chest deformity
- Oxygen saturation: Using a pulse oximeter on your finger
- General appearance: Signs of cyanosis (blue discoloration), weight loss, muscle wasting
- Heart examination: Checking for signs of heart strain
- Extremity examination: Looking for swelling in ankles or legs
Diagnostic tests
Spirometry (primary diagnostic test) – This is the gold standard for diagnosing COPD:
What it measures:
- FEV1 (Forced Expiratory Volume in 1 second): Amount of air you can forcefully exhale in one second
- FVC (Forced Vital Capacity): Total amount of air you can exhale after deep breath
- FEV1/FVC ratio: The key diagnostic measurement
How it’s performed:
- You breathe normally, then take a deep breath in
- You blow out as hard and fast as possible into a mouthpiece
- Usually repeated several times for accuracy
- May be done before and after bronchodilator medication
COPD diagnosis criteria:
- FEV1/FVC ratio < 0.70 (or 70%) after bronchodilator use
- This indicates persistent airflow limitation
COPD severity staging (GOLD classification):
Based on FEV1 percentage of predicted normal:
- GOLD 1 (Mild): FEV1 ≥ 80% predicted
- GOLD 2 (Moderate): 50% ≤ FEV1 < 80% predicted
- GOLD 3 (Severe): 30% ≤ FEV1 < 50% predicted
- GOLD 4 (Very Severe): FEV1 < 30% predicted
Chest X-ray
While not diagnostic for COPD, it helps:
- Rule out other lung conditions (lung cancer, pneumonia, heart failure)
- Detect signs of emphysema in advanced cases:
- Hyper-inflated (enlarged) lungs
- Flattened diaphragm
- Increased air spaces
- Identify bullae (large air pockets)
- Assess heart size
Chest CT scan (Computed tomography)
More detailed than X-ray and is useful for:
- High-resolution CT (HRCT): Shows detailed lung structure
- Detecting emphysema and its distribution pattern
- Identifying bullae that might need surgery
- Evaluating for lung cancer (smokers are at higher risk)
- Planning for lung volume reduction surgery or transplant
- Differentiating COPD from other lung diseases
Arterial blood gas (ABG) test
Measures oxygen and carbon dioxide levels in blood:
- Blood sample taken from artery (usually wrist)
- Shows how well lungs transfer oxygen to blood
- Indicates if you need supplemental oxygen
- Measures:
- PaO2: Partial pressure of oxygen
- PaCO2: Partial pressure of carbon dioxide
- pH: Blood acidity
- Oxygen saturation
- Typically done in severe COPD or during exacerbations
Pulse oximetry
- Simple, non-invasive test
- Clip placed on finger measures oxygen saturation
- Normal is 95-100%
- COPD patients may have lower readings (88-92%)
- Used for monitoring and determining oxygen therapy need
Alpha-1 antitrypsin deficiency screening
This blood test is recommended if:
- COPD develops before age 45
- COPD with minimal or no smoking history
- Family history of early COPD or liver disease
- COPD in non-smoker
- Emphysema in lower lobes (unusual pattern)
Exercise testing (6-minute walk test) to measure
- Distance walked in 6 minutes
- Oxygen saturation during exercise
- Symptom severity with exertion
- Response to oxygen therapy
- Helps assess:
- Disease severity
- Exercise capacity
- Need for pulmonary rehabilitation
- Prognosis
Sputum examination (analysis of mucus you cough up):
- Checks for bacterial infections
- Identifies organisms causing exacerbations
- Guides antibiotic selection
- Rules out tuberculosis or other infections
Electrocardiogram (ECG/EKG) (to measure the heart’s electrical activity):
- Detects heart problems related to COPD
- Identifies cor pulmonale (right-sided heart failure)
- Rules out heart disease causing symptoms
Echocardiogram (heart ultrasound) (used in advanced COPD):
- Assesses heart function
- Detects pulmonary hypertension
- Evaluates right ventricle function
- Helps guide treatment decisions
Additional assessments
Symptom questionnaires – standardised assessments include:
- CAT (COPD Assessment Test): 8-question survey scoring symptom impact
- mMRC (Modified Medical Research Council) Dyspnea Scale: Rates breathlessness severity
- BODE Index: Combines Body mass, Obstruction, Dyspnea, Exercise capacity for prognosis
Lung volume measurements – detailed pulmonary function tests:
- Total Lung Capacity (TLC): Often increased in COPD
- Residual Volume (RV): Air left after full exhalation (increased in COPD)
- Functional Residual Capacity (FRC): Air in lungs at rest
- Helps distinguish COPD from restrictive lung diseases
Diffusing capacity (DLCO) – measures how well lungs transfer gas:
- You inhale small amount of carbon monoxide
- Measures how much is absorbed
- Reduced in emphysema
- Helps assess severity of emphysema
Differential diagnosis
Your doctor will rule out conditions with similar symptoms:
- Asthma: Usually reversible airflow obstruction
- Congestive heart failure: Can cause shortness of breath
- Bronchiectasis: Chronic widening of airways
- Tuberculosis: Infectious disease
- Lung cancer: Especially in smokers
- Interstitial lung disease: Different pattern on imaging
- Obliterative bronchiolitis: Rare airway disease
Diagnosis process timeline
Typical diagnostic pathway:
- Initial visit: Medical history, physical exam, spirometry
- If spirometry shows obstruction: Chest X-ray, blood tests
- Confirmation visit: Repeat spirometry after bronchodilator
- Further testing: Based on severity and symptoms
- Ongoing monitoring: Regular spirometry to track progression
When to seek diagnosis
Get evaluated if you have:
- Chronic cough lasting more than 3 months
- Shortness of breath with normal activities
- Excess mucus production
- Wheezing or chest tightness
- History of smoking or occupational exposures
- Age 40+ with respiratory symptoms
- Frequent respiratory infections
Importance of early diagnosis
Early detection is crucial because:
- Treatment works best when started early
- Can slow disease progression
- Allows for smoking cessation intervention
- Prevents complications
- Improves quality of life
- Enables better disease management
Monitoring after diagnosis
Once diagnosed, regular monitoring includes:
- Spirometry: Every 6-12 months to track progression
- Symptom assessment: Each time you visit the docor
- Oxygen levels assessment: As needed
- Exacerbation frequency: Tracking flare-ups
- Imaging: Periodically or if symptoms worsen
- Complication screening: Heart function, bone density, mental health
Remember: If you have symptoms or risk factors for COPD, don’t wait. Early diagnosis and treatment can significantly improve outcomes and quality of life. Talk to your doctor about getting tested, especially if you’re a current or former smoker over age 40.
Treatment
Conventional treatment of chronic obstructive pulmonary disease
Treatment can’t cure COPD but it helps control symptoms and slow the progression from getting worse.
Stop smoking
- This is the single most important step.
- Doctors can help with nicotine replacement or prescription medication.
Inhaled medicines (bronchodilators and steroids)
- Short-acting bronchodilators (e.g. salbutamol, ipratropium) — give quick relief.
- Long-acting bronchodilators (e.g. tiotropium, formoterol) — keep airways open longer.
- Inhaled corticosteroids — reduce inflammation in airways.
- Combination inhalers — often used together for better control.
Pulmonary rehabilitation
This is a supervised program of exercise, breathing training and education to improve quality of life. Your doctor needs to refer you. To be eligible in Australia, your doctor needs to confirm you have been diagnosed with COPD. There are Medicare rebates.
Oxygen therapy
For people with very low oxygen levels and may be used at home.
- It helps people with severe breathing issues to breathe better.
- Improves life expectancy for those with severely low oxygen levels.
- Enhances quality of life when breathing becomes easier.
- Relieves breathlessness and makes normal activities more tolerable.
Surgery (in severe cases)
In severe cases, surgery may be required.
- Endobronchial valve replacement, a non surgical procedure, using a bronchoscope to insert valves into the damaged airways, to help with better breathing, increase exercise tolerance and improve quality of life.
- Lung volume reduction or bullectomy, which are are surgical procedures to remove damaged parts of the lung. This will decrease the volume of the lungs.
- Lung transplant, where a badly disease lung is replaced with a fresh, healthy lung. It is only for end-stage disease. This procedure will require lifelong medication to prevent organ rejection.
Vaccinations and antibiotics
- Flu and pneumonia vaccines prevent flare-ups.
- Antibiotics treat bacterial infections so they don’t cause worsening of COPD.
Alternative
Alternative / complementary treatment of chronic obstructive pulmonary disease
Complementary approaches may help relieve symptoms and improve wellbeing, but they don’t replace medical treatment. Always talk to your doctor before trying them as they can interact with medications.
Breathing exercises
These techniques can help you breathe better and reduce shortness of breath.
Pursed-lip breathing
This breathing exercise, helps you exhale air slowly and fully, preventing air from getting trapped in the lungs.
- How to do it: Inhale through your nose for two seconds, then exhale gently through pursed lips for four seconds.
- Benefits: Reduces shortness of breath and helps you stay calm.
Diaphragmatic (belly) breathing
This breathing exercise, helps to strengthen the main breathing muscle — the diaphragm.
- How to do it: Place a hand on your belly, breathe in deeply through your nose, letting your stomach rise, then exhale slowly.
- Benefits: Improves oxygen exchange and lung efficiency.
Pulmonary rehabilitation
Although considered mainstream, it includes many holistic elements: exercise training, nutrition advice and psychological support.
- Benefits: Improves stamina, reduces flare-ups, and helps manage anxiety about breathlessness.
Yoga and tai chi
Gentle exercise that improves breathing control, flexibility and relaxation.
- Evidence: Several studies shows it improve lung function, increases exercise tolerance and enhances mood in COPD patients.
- Tip: Choose slower, gentle forms to avoid strain.
Nutritional supplements
These can help to support lung health. Always consult a doctor before trying any supplements as they can interfere and react badly with your medications. Don’t stop taking medications to try supplements.
Omega-3 fatty acids
- Omega-3s are anti-inflammatory and directly help to reduce inflammation in the lungs.
- Some studies show they help ease breathing symptoms and reduce flare-ups.
- Studies suggest omega-3s can help improve physical performance and may help widen lung bronchiole for better breathing.
- Combat bacterial infections in the lungs to reduce the risk of flu and other respiratory infections.
- Found in salmon, sardines, mackerel, cod liver oil, oysters, caviar, herring, soybeans, flaxseed oil, chia seeds, flaxseeds, walnuts, hemp seeds, omega-3 enriched eggs, meat and dairy from grass fed animals, free range and organic eggs.
- Available as supplements – both as fish oil and plant based supplements.
- Typical dose for adults: 1,000–2,000 mg EPA/DHA per day (consult your doctor before taking them as they can adversely affect your medications).
Vitamin A
This antioxidant vitamin may protect the lungs from oxidative stress
- Helps to repair the lung cells and keep lungs healthy.
- Protects lungs from damage caused by smoking and other lung chemical irritants.
- Has anti-inflammatory properties which can help reduce inflammation in the lungs.
- Supports the immune system, which means fewer lung infections that happen less frequently.
- Some studies show people with COPD may be somewhat deficient in this vitamin so supplements may be needed.
- Found in liver (beef has the highest levels), fish (salmon, herring), cod liver oil, eggs, dairy (milk and cheese), vitamin A fortified foods. The following foods contain betacarotene, which is the precursor of vitamin A – orange and yellow vegetables (carrots, sweet potatoes, pumpkin, squash), dark green leafy vegetables (spinach, kale, greens), orange and yellow fruits (mango, melon, apricots, nectarines), red and green peppers/capsicum, tomatoes.
- Available as supplements – in tablet or capsule form, chewable and gummies.
- Typical dose for adults: 900mcg a day for men and 700mcg a day for women, tolerable upper limit 3,000mcg a day but this includes vitamin A from all sources, not just supplements. Don’t overdo it with this vitamin as it can be toxic at high doses. Smokers or former smokers should not take betacarotene, which is the precursor of vitamin A. Women who are pregnant or intending to get pregnant should not take high doses of vitamin A.
Vitamin C
This antioxidant vitamin may protect the lungs from oxidative stress
- Reduces inflammation in the lungs.
- Improves lung function and breathing.
- Powerful antioxidant that neutralises free radicals and other harmful elements in cigarette smoke to protect the lungs.
- Works synergistically with other antioxidants, which further protects the lungs.
- Some animal studies show vitamin C can prevent emphysema from developing and even help restore lungs damaged by COPD.
- Low levels of vitamin C is linked to many health conditions and to poorer lung function. Smokers deplete a lot of their vitamin C by smoking, so will need more in their diet.
- Found in berries, citrus fruits, leafy green vegetables,
- Available as supplements – in tablet or capsule form, chewable and gummies.
- Typical dose for adults: at least 400mg a day, tolerable upper limit 2,000mg a day and it’s recommended to take smaller doses in equal amounts at different times of the day (eg 1,000mg twice a day). Taking more than this can cause diarrhoea, stomach cramps and nausea.
Vitamin D
This hormone-like vitamin is essential for lung health.
- Reduces overall inflammation in the lungs.
- Boosts the immune system, which can help reduce the severity and length of respiratory infections.
- Prevents flare-ups, worsening of symptoms and hospitalisations.
- Improves lung function metrics, helps you breathe better.
- Supports muscle and bone health, prevents bone density loss and reduces the risk of osteoporosis.
- People with COPD have been found to be deficient in vitamin D and may require supplementation. A blood test is the best way to find out if you need this vitamin.
- Found in sunshine (richest sources), salmon, trout, mackrel, herrings, sardines, cod liver oil, egg yolks, beef liver, mushrooms, fortified foods.
- Available as supplements – in tablet or capsule form, chewable and gummies.
- Typical dose for adults: 15mcg-20mcg (600IU-800IU) per day, tolerable upper limit 100mcg (4,000IU) per day
Vitamin E
This antioxidant vitamin may protect the lungs from oxidative stress
- Boosts the immune system and helps reduce the severity and length of respiratory infections.
- Has an anti-inflammatory effect on the airways in the lungs, reducing mucous and unblocking airways.
- A study on people with COPD found that those with higher vitamin E intake in the diet have a lower risk of death from COPD.
- Vitamin E might be involved in preventing COPD from developing in the first place.
- The benefits of vitamin E seem to be due to dietary intake of foods high in this nutrient.
- Found in nuts and seeds (almonds, peanuts, sunflower seeds), vegetable oils (sunflower, safflower), green leafy vegetables, avocados, fortified foods.
- Available as supplements – in tablet or capsule form, chewable and gummies.
- Typical dose for adults: 15mg (22IU) per day, tolerable upper limit 100mcg (or 4,000IU) per day
Zinc
This antioxidant vitamin may protect the lungs from oxidative stress
- Reduces overall inflammation in the lungs.
- Boosts the immune system, which can help reduce the severity and length of respiratory infections.
- Helps the lungs cells walls to stay healthy and heal more quickly from damage.
- People with COPD often have low levels of zinc. A blood test is the best way to find out if you need this mineral.
- Found in oysters (richest source), beef, lamb, pork, chicken, turkey, crab, lobster, shellfish, milk, cheese, yoghurt, eggs.
- Available as supplements – in tablet or capsule form, chewable and gummies.
- Typical dose for adults: 14mg a day (men), 8mg a day (women), tolerable upper limit 40mg per day
Selenium
This antioxidant vitamin may protect the lungs from oxidative stress
- Reduces overall inflammation in the lungs.
- Boosts the immune system, which can help reduce the severity and length of respiratory infections.
- Studies show people with COPD (and smokers) who have higher blood selenium levels have better lung function and can breath more easily.
- In studies, people who received selenium, zinc, vitamin C and echinacea supplement showed less severe and shorter flare-ups.
- People with COPD often have low levels of selenium. A blood test is the best way to find out if you need this mineral.
- Found in Brazil nuts (richest source), tuna, oysters, halibut, organ meats, eggs, grains, legumes.
- Available as supplements – in tablet or capsule form, chewable and gummies.
- Typical dose for adults: 70mcg a day (men), 60mcg a day (women), tolerable upper limit 400mcg per day
Magnesium
This mineral is one of the most important ones for relaxing muscles and calming the mood.
- Helps to widen and relax airway muscles, which helps people breathe more easily. It’s a natural bronchodilator.
- Reduces overall inflammation in the lungs.
- Helps to relax muscles and helps COPD by relaxing the diaphragm to make it easier to breathe.
- People with COPD often have low levels of magnesium and in fact, low blood levels are a high risk factor for developing asthma and COPD as well as other lung conditions. A blood test is the best way to find out if you need this mineral.
- Magnesium sulfate (or sulphate) intravenously (into the vein with a needle) or inhaled is often used in hospitals as an extra treatment during acute COPD flare-ups to help with breathing
- Found in leafy green vegetables, almonds, cashews, peanuts, pumpkin seeds, chia seeds, legumes, whole grains, dark chocolate (at least 70%), salmon, milk, yoghurt, fortified foods.
- Available as supplements – in tablet or capsule form, chewable and gummies.
- Typical dose for adults: 400mg-420mg per day (men), 310mg-320mg per day, tolerable upper limit 350mg per day
Herbal options (with medical supervision)
Ginseng
Ginger has anti-inflammatory and antioxidant properties. Study results are mixed but this could be due to the type, amount and strength of ginseng used in the studies. More studies are needed to confirm any benefits for COPD.
Ginger
Ginger has potent anti-inflammatory and antioxidant properties that may support lung function and reduce inflammation.
Echinacea
Studies show echinacea supports and enhances the immune system. It may be beneficial to shorten the duration and intensity of respiratory infections.
Elderberry
Studies show elderberry may support immunity during infections. It may be beneficial to shorten the duration and intensity of respiratory infections.
Acupuncture
some studies show it can ease breathlessness and improve exercise tolerance.
Mind-body therapies
meditation and mindfulness reduce stress and improve coping.
Self care
Chronic obstructive pulmonary disease self care
Simple lifestyle actions can make a big difference:
Quit smoking completely
This is the single most important intervention to slow the progression of COPD. Some of the ways you can help yourself quit:
- Use nicotine replacement therapy (patches, gum, lozenges)
- Consider prescription medications that reduces your addiction to smoking (Varenicline, Bupropion)
- Join support groups or counselling programs for quitting smoking
- Avoid secondhand smoke
Exercise regularly
Even gentle walking strengthens the lungs.
- Walking – start with short distances and gradually increase the distance you walk, as much as you can handle with your doctor’s approval
- Stationary cycling is a low-impact cardiovascular exercise
- Arm exercises strengthen upper body muscles and help lungs. You can even do these sitting down
- Stretching helps to maintain flexibility
- Aim for 30 minutes of exercise every day, as tolerated
Eat a balanced, healthful diet
Make sure to eat mostly fresh, unprocessed foods.
- Try to eat smaller, more frequent meals (5-6 per day)
- High-protein diet supports muscle maintenance. Just make sure you are also eating protein from plant sources too
- Prevent weight loss and muscle wasting by having adequate calories
- Limit adding too much salt to food or eating processed foods, which contain a lot of salt. Reducing salt in your diet reduces fluid retention
- Stay hydrated with 6-8 glasses of water daily
- Avoid gas-producing foods (broccoli, beans, cabbage) as they can cause bloating and breathing difficulty
Maintain a healthy weight
Too much or too little can make breathing harder.
- Check your BMI to ensure you are not in the obese range
- Lose weight if you need to and discuss your plans with your doctor and a dietician
- Make sure you get enough unprocessed foods in your diet
- Eat the right proportions of protein, carbohydrates and fats in your meals
Get enough rest
Maintain good sleep hygiene.
- When symptoms are worse, try to sleep with your head elevated by using 2-3 pillows
- Maintain a regular sleep schedule most nights
- Address sleep apnea if present – talk to your doctor about strategies and tools
- Avoid eating large meals before bed as this can make it difficult to breath properly for well people, nevertheless for anyone with COPD
Manage stress
There can be a lot of stress when living with a chronic disease.
- Practice relaxation techniques
- Join support groups
- Maintain social connections – join interest groups
- Seek counselling if you are experiencing depression or anxiety
Avoid triggers and environmental chemicals
Avoid anything that irritates your airways and makes breathing more difficult:
- Avoid air pollutants such as smoke, dust, fumes, chemicals, strong cleaning products, perfumes
- Monitor air quality outside and stay indoors on high pollution days
- Use air purifiers at home
- Maintain proper humidity in your home to ensure the air is not dry. Good humidity is around 30%-50%
- Avoid extreme temperatures
Follow your medication plan
Take the medications your doctor prescribes exactly as they recommend. This will help reduce the incidence of flareup.
- Learn proper inhalers intake techniques
- Keep your medications refills in a safe place so you can get refills when you need them
- Monitor any side effects and discuss them with your doctor or specialist
- Don’t skip medicines
Monitor symptoms
Check on your symptoms regularly.
- Track symptoms daily – use a symptom diary to note any changes in symptoms. There are many apps that do this for free
- Monitor your lungs peak flow if you are advised to do so
- Recognise exacerbation signs: increased breathlessness, cough, mucus changes
- Have an action plan: Know when to call the doctor
- Regular follow-ups with healthcare providers
- If your breathlessness suddenly worsens, seek medical help quickly.
Infection prevention
Try to stay germ free as infections can exacerbate symptoms and cause flare-ups.
- Wash your hands frequently if you’re out of the home and if you can’t wash them, use sanitiser that has at least 70% alcohol
- Avoid crowds, crowded places, public transport, shops during flu season
- Stay up-to-date on vaccinations
- Maintain good oral hygiene by brushing your teeth twice a day and flossing regularly
Energy conservation
When symptoms cause issues with daily activities, take your time and conserve your energy.
- Pace yourself and rest between activities, especially if it makes breathing more difficult
- Use assistive devices if you need them – this includes shower chairs, reaching tools
- Keep frequently used items within easy reach
- Sit while working when possible
- Coordinate breathing with activities
Stay connected
Join both online and in-person support groups or talk with others living with COPD. This will help you feel less alone and more connected to others experiencing the same illness as you.
References
References
- Agustí A, Hogg JC. Update on the pathogenesis of chronic obstructive pulmonary disease. N Engl J Med. 2019;381(13):1248–1256.
- American Thoracic Society/European Respiratory Society. (2004). Standards for the Diagnosis and Management of Patients with COPD.
- Anthonisen NR, et al. (1994). The effects of a smoking cessation intervention on 14.5-year mortality: a randomized clinical trial. Annals of Internal Medicine, 142(4), 233-239.
- Australian Lung Foundation. Chronic obstructive pulmonary disease (COPD). Accessed 11 November 2025
- Barnes, P.J., et al. (2015). Chronic obstructive pulmonary disease. Nature Reviews Disease Primers, 1, 15076.
- Bourbeau J, et al. (2003). Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management intervention. Archives of Internal Medicine, 163(5), 585-591
- Calverley PM, et al. (2007). Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. New England Journal of Medicine, 356(8), 775-789.
- Casaburi R, ZuWallack R. Pulmonary rehabilitation for management of chronic obstructive pulmonary disease. N Engl J Med.
- Celli BR, Wedzicha JA. Update on clinical aspects of chronic obstructive pulmonary disease. N Engl J Med. 2019;381(13):1257–1266.
- Criner GJ, Bourbeau J, Diekemper RL, et al. Prevention of acute exacerbations of COPD. Chest. 2015;147(4):894–942.
- Fishman A, et al. (2003). A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. New England Journal of Medicine, 348(21), 2059-2073.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2024 report.
- Hirayama F, Lee AH, Oura A, et al. Dietary intake of fish and n-3 fatty acids and chronic obstructive pulmonary disease mortality: a population-based prospective study. Nutr Metab Cardiovasc Dis. 2009;19(10):716–722.
- Li M, Yang H, Zhang Y, et al. Acupuncture for chronic obstructive pulmonary disease: a systematic review and meta-analysis. Complement Ther Med. 2015;23(4):585–595.
- Liu X, et al. (2014). Ginseng on hyperglycemia: effects and mechanisms. Evidence-Based Complementary and Alternative Medicine, 2014, 696508.
- Long Term Oxygen Treatment Trial Research Group. (2016). A randomized trial of long-term oxygen for COPD with moderate desaturation. New England Journal of Medicine, 375(17), 1617-1627.
- Martineau AR, et al. (2015). Vitamin D for the management of asthma and COPD. Cochrane Database of Systematic Reviews, (5), CD011511.
- National Institute for Health and Care Excellence (NICE). (2019). Chronic obstructive pulmonary disease in over 16s: diagnosis and management. NICE guideline [NG115].
- Ng BH, et al. (2014). Functional and psychosocial effects of health qigong in patients with COPD: a randomized controlled trial. Journal of Alternative and Complementary Medicine, 20(4), 243-253.
- Ngai SP, et al. (2016). Effects of tai chi on chronic obstructive pulmonary disease: a systematic review. Complementary Therapies in Medicine, 26, 96-104.
- Nici L, et al. (2006). American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. American Journal of Respiratory and Critical Care Medicine, 173(12), 1390-1413.
- O’Donnell DE, Laveneziana P. Dyspnea and activity limitation in COPD: mechanical factors. COPD. 2007;4(3):225–236. 2009;360(13):1329–1335.
- Rabe KF, Watz H. Chronic obstructive pulmonary disease. Lancet. 2017;389(10082):1931–1940.
- Rennard SI, Drummond MB. Early chronic obstructive pulmonary disease: definition, assessment, and prevention. Lancet. 2015;385(9979):1778–1788.
- Ries AL, et al. (2007). Pulmonary rehabilitation: joint ACCP/AACVPR evidence-based clinical practice guidelines. Chest, 131(5 Suppl), 4S-42S
- Singh D, Agusti A, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2019 report. Eur Respir J. 2019;53(5):1900164.
- Steiner MC, et al. (2005). Nutritional enhancement of exercise performance in chronic obstructive pulmonary disease: a randomised controlled trial. Thorax, 58(9), 745-751.
- Stey C, et al. (2000). The effect of oral N-acetylcysteine in chronic bronchitis: a quantitative systematic review. European Respiratory Journal, 16(2), 253-262.
- Suzuki M, et al. (2016). A randomized controlled trial of acupuncture in patients with chronic obstructive pulmonary disease (COPD). Archives of Internal Medicine, 172(11), 878-886.
- Tashkin DP, et al. (2008). A 4-year trial of tiotropium in chronic obstructive pulmonary disease. New England Journal of Medicine, 359(15), 1543-1554
- Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of COPD. Am J Respir Crit Care Med. 2013;187(4):347–365.
- Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. Am J Respir Crit Care Med. 2017;195(5):557–582.
- Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796.
- Wongsurakiat P, Maranetra KN. Role of nutritional support in chronic obstructive pulmonary disease. J Med Assoc Thai. 2004;87(3):292–299.
Last reviewed and updated: 12 November 2025