Facts
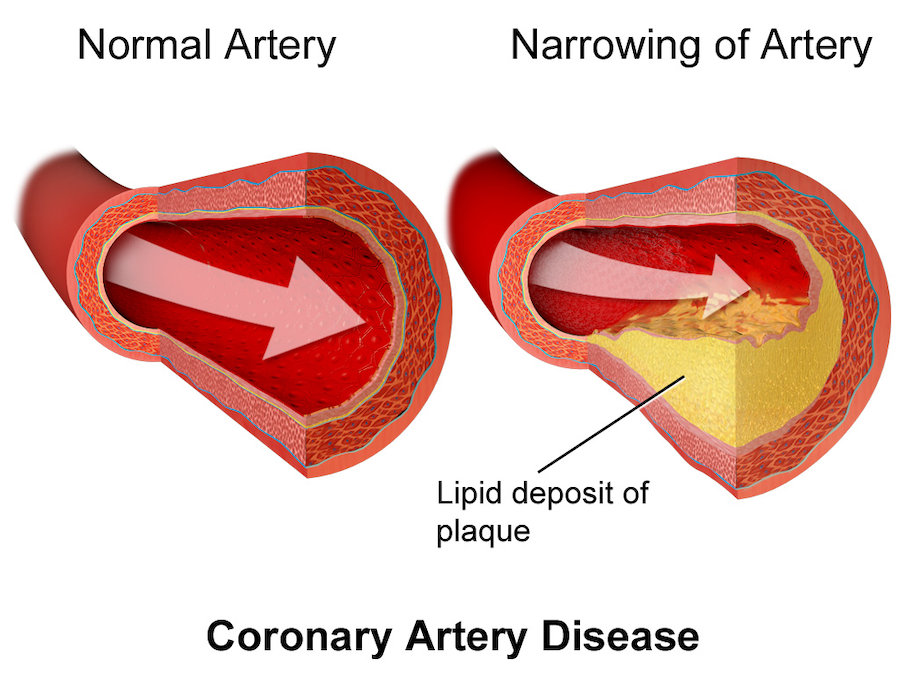
Coronary artery disease (CAD) occurs when the coronary arteries that supply blood to the heart muscle become narrowed or blocked, most commonly due to atherosclerosis — the buildup of cholesterol, fatty deposits (plaques), and inflammatory cells on the arterial walls. This process can lead to reduced oxygen delivery to the myocardium (heart muscle), causing angina, heart attack (myocardial infarction), and potentially heart failure if untreated.
CAD is the leading cause of death worldwide, responsible for around 17.9 million deaths per year globally (WHO, 2023).
CAD starts with the cells lining the blood vessels (endothelial cells) becoming damaged and unhealthy. This leads to impaired blood vessels. Smoking, high blood pressure, high LDH cholesterol, diabetes, obesity can all contribute to CAD developing.
When the inner lining of your blood vessels (called the endothelium) gets damaged — from things like smoking, high blood pressure, or too much cholesterol — it becomes a bit “leaky.” This lets bad cholesterol (LDL) slip into the wall of the artery.
Once inside, that cholesterol becomes damaged by oxygen (oxidised), which makes it harmful. The body sees this as a problem and sends in white blood cells (called macrophages) to clean it up. But instead of fixing the issue, the white blood cells fill up with the fatty cholesterol and turn into foam cells — like little fat-filled bubbles.
Over time, these foam cells pile up and form fatty streaks along the artery wall. As the process continues, more fat, cells and scar tissue build up, creating a plaque. This is a thick, hard lump that can narrow the artery and slow down blood flow to your heart, brain, lungs or other parts of your body.
As plaques grow, they narrow blood vessels or arteries, which reduces blood flow. If a plaque burst in the blood vessel, it triggers the body to form a blood clot at the rupture site as a way to repair the damage. This can lead to life-threatening blockage of the artery.
- If the rupture happens in a coronary artery (one of the blood vessels going to the heart), it can cause a heart attack
- It the rupture happens happens in an artery supplying blood to the brain, it can cause a stroke
- If the rupture happens happens on other arteries, it can still be very dangerous
All of these require immediate medical attention. Call an ambulance 000.
Symptoms
Symptoms of coronary artery disease
The first common symptom of coronary artery disease often include:
- chest pain or discomfort (angina), which can feel like pressure, squeezing, heaviness, burning or tightness in the chest area
Other common initial symptoms are:
- Shortness of breath – feeling like you can’t breathe properly
- Pain or discomfort in other body areas – pressure or pain in other parts of the body, particularly the upper arms, back, jaw, neck or stomach
- Fatigue – extreme tiredness for no reason
- Dizziness – feeling lightheaded or unsteady on your feet
- Cold sweats – suddenly feeling very cold for no reason (for example, it isn’t really cold or you don’t have an infection)
- Nausea – feeling sick in your stomach
- Silent ischaemia – people with diabetes may experience reduced blood flow to the heart but no chest pain, as their nerve damage masks pain. Their lack of symptoms can delay treatment until CAD has progressed to a serious level
These symptoms can indicate another health condition, so always consult your medical doctor if you’re experiencing any of these symptoms. Always call an ambulance if you suspect you’re having a heart attack. It’s better to have a false alarm than the alternative.
Causes
Causes of coronary artery disease
There are a number of risk facts that are associated with coronary artery disease:
- High LDL cholesterol and low HDL cholesterol
- High blood pressure (hypertension)
- Smoking
- Diabetes
- Obesity and other metabolic syndromes
- Physical inactivity
- Poor diet (high in processed foods, refined carbohydrates and salt)
- Chronic stress and depression
- Excessive alcohol consumption
- Being over 45 if you’re a man or over 55 if you’re a woman, post-menopausal
- Family history of heart disease
Prevention
Prevention of coronary artery disease
Strategies you can use to reduce your risk of coronary artery disease – not everyone of these strategies applies to every person:
- Stop smoking or don’t start in the first place – tobacco smoke both from smoking and second hand smoke, is one of the biggest risk factors
- Eat more unprocessed, fresh food – get more fresh fruit, vegetables, legumes, whole grains, nuts, seeds and good fats in your diet
- Reduce alcohol intake – alcohol is another big risk factor for this disease. The World Health Organisation (WHO) recommends no more than 10 alcoholic drinks a week, but they advise that any amount of alcohol can be harmful. WHO states that no amount of alcohol is considered safe for pregnant or breastfeeding women, who should not be drinking any alcohol
- Get active – the Australian government recommends adults should be physically active preferably every day, with up to 5 hours of moderate physical activity and up to 2.5 hours of vigorous physical activity each week
- Reduce your LDL cholesterol levels – if you have high LDL cholesterol levels, make sure you are taking the right steps to reduce it to healthier levels
- Manage your diabetes – while diabetes type 1 is an autoimmune condition and diabetes type 2 is due to lifestyle factors, both can benefit from management. Both are mostly manageable with a good diet, adequate exercise and medication
- Lose weight – if you are even moderately overweight, you need to try to lose weight. See a dietician for help with dietary recommendations to help you eat well
- Manage menopause – women over 50 who are experiencing menopause symptoms should ensure they have a healthy diet, reduce stress and avoid hot flashes triggers. Medication may be required for some women but they should consult with a doctor for individual advice tailored to their specific situation
- Talk to your doctor about your risks – always talk to your doctor if you have any of the risk factors
Complications
Complications of coronary artery disease
Coronary artery disease doesn’t just cause chest pain or tiredness. It can lead to serious and sometimes life-threatening problems when blood flow to the heart muscle becomes too restricted or completely blocked.
The complications depend on how severe the blockages are and how long the heart muscle is deprived of oxygen.
Angina pectoris (chest pain)
When your heart muscle doesn’t get enough oxygen during exertion, stress, or cold exposure, it causes pain or pressure in the chest (sometimes spreading to the arm, neck, or jaw). There are 3 types of angina:
- Stable angina – Predictable pain that occurs with activity and eases with rest or nitroglycerin.
- Unstable angina – New or worsening pain that occurs at rest or with minimal effort — a medical emergency, as it may precede a heart attack.
- Variant (Prinzmetal’s) angina: – Caused by temporary artery spasm, not plaque.
Angina is an early warning sign that your heart isn’t getting enough oxygen and needs medical attention to prevent more serious complications.
Heart attack (myocardial infarction)
A plaque in a coronary artery ruptures, causing a blood clot (thrombus) that suddenly blocks blood flow to part of the heart muscle.
The heart muscle begins to die (infarct) from lack of oxygen.
Symptoms
- Crushing chest pain
- Sweating
- Shortness of breath
- Nausea
- Light-headedness
Quick treatment is critical — within 90 minutes if possible — to restore blood flow and limit damage.
If untreated, a heart attack can lead to heart failure, arrhythmias or death.
Heart failure
When parts of the heart muscle are damaged or weakened by repeated lack of oxygen (or a large heart attack), the heart can’t pump blood very well. Over time, the heart enlarges and becomes less efficient, leading to chronic breathlessness and reduced quality of life.
Symptoms
- Shortness of breath
- Fatigue
- Swelling in the legs or ankles
- Difficulty lying flat
CAD is the most common cause of heart failure worldwide.
Arrhythmias (abnormal heart rhythms)
Abnormal heart rhythms can be caused by damaged heart muscle or electrical pathways from CAD. This can disrupt the heart’s normal rhythm. There are a few types of arrhythmias:
- Atrial fibrillation (AF) – irregular heartbeats that increase stroke risk.
- Ventricular tachycardia (VT) – a life-threatening abnormal heart rhythm that can cause sudden heart attack and death.
- Ventricular fibrillation (VF) – a life-threatening rhythms that can cause sudden cardiac death.
The risk of arrhythmias increase after a heart attack or when the heart’s pumping function (ejection fraction) is reduced.
Sudden cardiac arrest
The heart suddenly stops beating effectively, often due to ventricular fibrillation after a heart attack or severe arrhythmia.
Without immediate cardiopulmonary resuscitation (CPR) or defibrillation, sudden cardiac arrest is fatal within minutes.
CAD is the leading cause of sudden cardiac death in adults.
Cardiogenic shock
When a large portion of the heart muscle is damaged (usually after a major heart attack), the heart can’t pump enough blood to supply vital organs.
Symptoms
- Rapid breathing
- Weak pulse
- Low blood pressure
- Confusion
- Cold, clammy skin
This is a medical emergency with high mortality unless treated rapidly in an intensive care unit.
Pericarditis (inflammation of the lining of the heart)
The sac around the heart (pericardium) becomes inflamed, sometimes after a heart attack — known as Dressler’s syndrome.
Symptoms
- Sharp chest pain that worsens when lying down or breathing deeply.
Pericarditis can cause pericardial effusion (fluid around the heart), restricting its pumping ability if severe.
Ventricular aneurysm
After a large heart attack, part of the weakened heart wall bulges outward, forming an aneurysm in a ventricle.
It can lead to heart failure, arrhythmias or blood clots inside the aneurysm that may cause stroke.
Stroke and peripheral vascular disease
CAD and atherosclerosis often adversely affect the function and health of other arteries too — in the brain and legs.
- Stroke: Plaque rupture or blood clots can travel to brain arteries, blocking blood flow and causing a stroke.
- Peripheral artery disease (PAD): Narrowing in leg arteries causes pain while walking (claudication).
These conditions share the same root cause — atherosclerosis — and increase overall cardiovascular risk.
Emotional and psychological complications
After a heart attack or diagnosis of CAD, many people experience anxiety, depression or fear of exertion.
Emotional stress can worsen symptoms, increase heart rate and blood pressure and affect recovery.
Cardiac rehabilitation and psychological support significantly improve long-term outcomes.
Diagnosis
Diagnosis of coronary artery disease
Your doctor will diagnose your condition through:
Medical history and risk assessment
Your doctor starts by asking questions to understand your symptoms and risk factors, such as:
- Chest pain or discomfort (angina) – when it happens, how long it lasts, and what brings relief
- Shortness of breath, fatigue, or dizziness
- Family history of heart disease
- Lifestyle factors (smoking, diet, activity level, alcohol use)
- Existing conditions such as diabetes, high blood pressure, or high cholesterol
This information helps the doctor estimate your likelihood of having CAD before ordering further tests.
Physical examination
A physical exam may include:
- Listening to the heart for abnormal sounds (murmurs or irregular rhythms)
- Checking blood pressure and pulse in different areas
- Examining for signs of poor circulation, such as cool skin, weak pulses or swelling
- Looking for cholesterol deposits under the skin or around the eyes (xanthomas)
These physical clues can suggest how well your heart and cardiovascular system is working.
Blood tests
Blood tests help identify risk factors and detect evidence of heart stress or injury.
Lipid profile
This test checks total cholesterol, LDL (bad), HDL (good), triglycerides. It’s important to see if there is high LDL cholesterol as it increases risk of plaque buildup.
High-sensitivity C-reactive protein (hs-CRP)
This test measures the level of inflammation in the body. It’s a good all-round test to check for any type of inflammatory illness. Chronic inflammation contributes to coronary artery disease and atherosclerosis.
Blood glucose / HbA1c
This test checks for diabetes or pre-diabetes as diabetes can speed up artery plaque damage.
Troponin
This is a cardiac enzyme. It is released after
- heart muscle damage
- a blood clot in the lungs (pulmonary embolism)
Blood clots don’t release troponin – it is a protein found in heart muscle cells. It is the strain and potential damage to the heart caused by the clot that leads to the release of troponin.
Kidney function & electrolytes
This test checks overall health and is important before any imagine or medications are prescribed. It may also be prescribed if certain heart medications are taken, as they can potentially damage the kidneys.
Electrocardiogram (ECG or EKG)
- Abnormal heart rhythms (arrhythmias)
- Evidence of past or current heart attacks
- Reduced blood flow to the heart (ischaemia)
An ECG is often the first test if your doctor thinks you might have CAD as it’s quick, painless and non-invasive.
Echocardiogram (heart ultrasound)
- The heart structure (valves, upper and lower chambers)
- How well your heart pumps blood (ejection fraction)
- Areas of weak or damaged heart muscle (from poor blood flow)
This test is very useful as it can identify heart damage caused by reduced oxygen from blocked arteries.
Cardiac stress test
- Detects reduced blood flow to the heart under stress
- Helps reveal blockages that may not appear at rest
There are several types of cardiac stress tests. In all of these test, you have small sticky patches (electrodes) are placed on your chest, arms, and legs to record heart signals:
- Exercise ECG stress test – where you are Measures heart rhythm during physical activity.
- Stress echocardiogram – takes ultrasound images before and after exercise.
- Nuclear stress test – uses a safe radioactive tracer and a camera to show blood flow to the heart.
Coronary CT angiography (CCTA)
- The presence, size, and location of plaques
- Whether arteries are narrowed or blocked
CCTA is non-invasive and often used to rule out CAD in people with moderate risk or unclear test results.
Coronary angiography (cardiac catheterisation)
- A thin tube (catheter) is inserted through an artery in your wrist or groin.
- A contrast dye is injected into your coronary arteries.
- X-ray images show where and how much narrowing in the arteries exists.
If a blockage is found, a stent can sometimes be placed while this test is being performed to open the artery (angioplasty). Your doctor will explain all the details and the risks of the test before you do it.
Because this test is invasive, it’s usually reserved for people with strong evidence of CAD or severe symptoms.
Additional or specialised tests
Sometimes more tests are used to assess overall heart health or plaque buildup:
- Coronary calcium scoring (CT scan) – this test measures calcium deposits in coronary arteries. Higher scores mean more plaque build-up and greater CAD risk. In this test, electrodes are placed on your body. You will lie on a table that slides into a circular CT scanner, which will take images while you hold your breath for short durations
- Cardiac MRI – this test provides detailed pictures of your heart structure and function without radiation. In this test you will be lying on a table that slides into a large tunnel-like machine. You may or may not receive an intravenous (needle into your arm) with a contrast dye. You will be given ear plugs or headphones as the MRI machine is very loud. You cannot have this test if you have a pacemaker or any other metal in your body
- Ankle-brachial index (ABI) – this test is done by putting a blood pressure cuff on your arm and ankle, then measuring blood pressure in each. Your doctor will use a handheld ultrasound device to listen to your pulse to determine the exact point when the blood flow returns, providing the systolic pressure readings. The ABI is calculated by dividing the highest ankle pressure by the highest arm pressure, giving a ratio that indicates the severity of peripheral artery disease
Prognosis
Treatment
Conventional treatment of coronary artery disease
The conventional treatment of coronary artery disease is based on lifestyle changes and taking certain medicines. Surgery may be needed for severe cases.
Lifestyle
Changes to your lifestyle is the one biggest factor to reducing your risk of coronary artery disease or reducing it from worsening.
Heart-healthy diet
- Mediterranean diet – rich in fruits, vegetables, legumes, nuts, olive oil, and fish.
Evidence: Reduces cardiovascular events by ~30% in high-risk populations (PREDIMED study, Estruch et al., 2013). - DASH diet – reduces blood pressure and improves lipid profiles.
Plant-based diets – shown to reduce LDL cholesterol and atherosclerosis progression (Ornish et al., 1998).
Omega-3 fatty acids (EPA/DHA) – reduce triglycerides, inflammation, and platelet aggregation.
Physical activity
- At least 150 minutes a week of moderate-intensity aerobic exercise.
- Improves blood vessel function, lowers blood pressure and insulin resistance and raises HDL (good cholesterol).
Stress management
Yoga, meditation and mindfulness reduce stress hormones and may improve blood vessels
Stop smoking
Within one year of quitting, CAD risk drops by about 50%.
Weight management
- BMI goal: 18.5–24.9 kg/m²
- Waist circumference should be <94 cm (men) or <80 cm (women).
Medicine
You can be prescribed one medicine or a combination, depending on your symptoms and disease progression.
Anti-platelet medicines
- They help to prevent blood clots by thinning the blood
- Examples – Aspirin, Clopidogrel, Prasugrel, Ticagrelor
Statins
- They lower LDL cholesterol and stabilise plaques
- Examples – Lipitor (atorvastatin), Crestor (rosuvastatin), Zocor (simvastatin), Pravachol (pravastatin)
ACE inhibitors / ARBs
- They reduce blood pressure and improve artery and blood vessel function
- Examples – Lisinopril, Enalapril, Ramipril, Benazepril, Captopril, Fosinopril, Moexipril, Perindopril, Quinapril, Trandolapril
Beta blockers
- They reduce heart rate, lower blood pressure and oxygen demand
- Examples – Metoprolol, Bisoprolol
Nitrates
- They dilate (open up) vessels, relieve angina pain and discomfort symptoms
- Examples – Glyceryl trinitrate
Calcium channel blockers
- They lower blood pressure, slow the heart, relax blood vessels and slow heart rhythm
- Examples – Amlodipine, Diltiazem
Surgery
When the arteries supplying the heart (coronary arteries) become too narrow or blocked, blood can’t reach the heart muscle properly. If this causes severe chest pain (angina), shortness of breath, or a heart attack, procedures are used to open or bypass the blocked arteries.
There are two main types of procedures:
- Percutaneous Coronary Intervention (PCI) – also called angioplasty with stenting
- Coronary Artery Bypass Grafting (CABG) – open-heart surgery to reroute blood flow
Percutaneous coronary intervention (PCI) – Coronary angioplasty or balloon angioplasty with stent placement
PCI is a minimally invasive surgical procedure to help open up narrowed or blocked coronary arteries. It’s performed in a hospital by a specialist cardiologist.
How it’s done (step by step)
- Preparation:
You’re given a sedative (you stay awake but relaxed). The doctor numbs your wrist or groin area. - Catheter insertion:
A thin flexible tube (catheter) is inserted into a blood vessel in your wrist (radial artery) or groin (femoral artery) and guided up to the heart. - Imaging and dye injection:
A contrast dye is injected to make the arteries visible on X-ray. This is called coronary angiography. - Balloon inflation:
A small balloon at the tip of the catheter is positioned inside the narrowed artery and then gently inflated.
This pushes the fatty plaque against the artery wall, widening the vessel and improving blood flow. - Stent placement:
A stent (a tiny mesh tube) is usually placed at the site of the blockage to keep the artery open permanently.
Bare-metal stents (BMS): early type, rarely used now.
Drug-eluting stents (DES): coated with medicine to prevent scar tissue and re-narrowing — now the standard choice. - Completion:
The balloon is deflated and removed, but the stent stays in place. The blood flow through the artery is restored almost immediately.
Recovery
- Hospital stay: usually 1 day.
- Light activity after a few days
- Full recovery in 1–2 weeks.
- You’ll take blood thinning (anti-platelet) medication (aspirin + clopidogrel) to prevent clots forming inside the stent.
Benefits
- Relieves chest pain (angina)
- Improves blood flow to the heart
- Reduces the risk of heart attack
- Short recovery time compared to surgery
Risks (generally low)
- Bleeding or bruising at catheter site
- Re-narrowing (restenosis) of artery (much less common with modern stents)
- Rare complications: heart attack, stroke, or need for emergency surgery
When PCI is used
- One or two blocked arteries
- Stable or unstable angina
- During a heart attack to quickly restore blood flow (emergency PCI)
Coronary artery bypass grafting (CABG) – Heart bypass surgery
CABG is a major surgical procedure performed when there are multiple blockages, complex plaque patterns or when PCI isn’t suitable.
The surgeon creates a new route (“bypass”) for blood to flow around the blocked arteries, supplying oxygen-rich blood to the heart muscle.
How it’s done (step by step)
- Anaesthesia and Preparation:
You’re given general anaesthesia (asleep during the operation). - Harvesting the Grafts:
The surgeon takes healthy blood vessels (called grafts) from other parts of your body:
– Saphenous vein from the leg
– Internal mammary artery from the chest wall
– Radial artery from the arm - Bypass Creation:
The surgeon connects one end of the graft above the blockage in the coronary artery and the other end below it.
This creates a new pathway for blood to flow to the heart muscle. - Heart-Lung Machine (in most cases):
During surgery, your blood may be circulated by a heart-lung machine while the heart is temporarily stopped.
(In “off-pump” CABG, the heart keeps beating during the procedure.) - Closing the Chest:
Once the grafts are in place, the chest is closed with sutures or staples.
Recovery
Hospital stay: usually 5–7 days.
Full recovery: 6–12 weeks, depending on your health and surgery type.
You’ll continue medications for blood pressure, cholesterol, and to protect grafts from clotting.
Benefits
Excellent long-term symptom relief
Improves blood flow to all affected heart areas
Reduces the risk of future heart attacks
Proven to extend survival, especially in people with left main coronary artery disease, multiple blocked arteries, diabetes
Risks
Bleeding or infection (especially in diabetic or older patients)
Stroke (small risk due to surgery)
Irregular heart rhythms (usually temporary)
Memory or concentration issues for a short time
Graft closure over time (most last 10–15+ years)
When CABG Is Used
Severe multi-vessel CAD (especially involving 3 or more arteries)
Blockage in the left main coronary artery (the artery supplying most of the heart muscle)
Failed previous PCI/stent
Patients with diabetes or poor heart function (CABG often gives better long-term results than stenting in these cases)
Other and emerging procedures
- Atherectomy – in this procedure a tiny rotating blade or laser is used to remove plaque buildup from artery walls. It’s used for very hard, calcified plaques where stents can’t expand the artery and blood vessel walls to allow better blood flow
- Coronary laser therapy – where laser light vaporises plaque blockages. This procedure is sometimes done before placing stents
- Hybrid coronary revascularisation – this procedure combines CABG (for major blockage) with PCI (for smaller arteries). It is only done on selected patients with multiple types of blockages
- Robotic or minimally invasive CABG – this procedure uses small incisions and robotic tools instead of full open-heart surgery. It means faster recovery and less pain, but available only in specialised centres and more costlier
Alternative
Alternative / complementary treatment of coronary artery disease
Do not stop taking any of your medications. Always consult your doctor about any supplements as they should not replace prescription medications
The best known and evidence based supplements to support your heart to help improve heart function, reduce symptoms and prevent further plaque build-up. They should be used only under the guidance of a doctor.
Coenzyme Q10 (CoQ10)
CoQ10 is a vitamin-like compound naturally made in the body. It helps cells produce energy and acts as an antioxidant, protecting blood vessels and heart tissue from damage.
Ensure you take the ubiquinol format at that is the one that is better absorbed by the body.
How it helps the heart
- Improves energy production in heart cells
- Reduces inflammation and damage in arteries
- May help reduce muscle ache side effects of statins
- Helps to improve heart function in people with heart failure or CAD
Evidence
- A large analysis of many studies found CoQ10 reduced death from all cause in people with heart failure and improved cardiac output.
- Another study showed improved function in the artery’s ability to relax and widen.
Typical dose
100–200 mg daily (taken with food for better absorption).
Omega-3 fatty acids (EPA and DHA)
Omega-3s are essential fats found in fish oils and some plants (like flaxseed and chia). The main heart-protective types are EPA and DHA.
How they help the heart
- Lower blood fats (triglycerides)
- Reduce inflammation in the artery walls, which reduces damage to them
- Improves the flexibility of blood vessels, which means they’re more open and allow better blood flow
- Helps to prevent blood clots and arrhythmias
- May slow the atherosclerosis from getting worse
Evidence
- The REDUCE-IT trial found that a purified EPA supplement reduced heart attack and stroke risk by 25% in high-risk patients already on statins.
- Other studies show consistent triglyceride reduction of 20–50%.
Typical dose
- For general heart health: 500–1000 mg/day EPA + DHA
- For high triglycerides: 2000–4000 mg/day (but only under medical supervision)
Magnesium
A vital mineral for muscle and nerve function, blood pressure regulation, and heartbeat rhythm.
How it helps the heart
- Helps relax blood vessels, improving blood flow
- Reduces high blood pressure
- Supports normal heart rhythm and prevents arrhythmias
- May reduce risk of sudden cardiac death
Evidence
- Large population studies show people with higher magnesium intake have lower CAD risk.
- Magnesium supplementation can reduce blood pressure in hypertensive patients.
Typical dose
200–400 mg/day (as magnesium citrate, glycinate or malate). Don’t use magnesium oxide as it is not well absorbed by the body.
Garlic (Allium sativum)
Garlic has long been used for heart health and has natural cholesterol-lowering and anti-clotting effects.
How it helps the heart
- Lowers LDL (“bad”) cholesterol
- Raises HDL (“good”) cholesterol slightly
- Reduces high blood pressure
- Acts as a natural blood thinner, reducing clot risk
- Contains antioxidants that protect arteries from damage
Evidence
- An analysis of a large number of studies found garlic supplements reduced total cholesterol by up to 10–15 mg/dL.
- May lower systolic blood pressure by 5–10 mmHg.
Typical dose:
- 600–1200 mg/day aged garlic extract
- Equivalent to 1 clove of raw garlic per day
Green tea catechins
Green tea is rich in catechins (especially EGCG), powerful antioxidants that support blood vessel health.
How it helps the heart
- Lowers LDL cholesterol and triglycerides
- Improves artery flexibility so that blood can flow more easily
- Reduces oxidative stress, which means it reduces the risk of damage to the artery walls
- May reduce plaque buildup and lower blood pressure
Evidence
- Meta-analyses show green tea drinkers have a 20–30% lower risk of heart disease.
- Catechins also reduce LDL oxidation, which is how atherosclerosis starts. This means it reduces the risk of hardened arteries where blood flow is poor.
Typical intake
- 3–4 cups/day or 250–500 mg extract.
- Make sure it’s from organic, untainted sources.
Pomegranate
A fruit high in polyphenols (especially punicalagins), which act as strong antioxidants.
How it helps
- Reduces oxidative stress in arteries
- Lowers LDL cholesterol oxidation
- Improves blood vessel function
- May slow plaque buildup
Evidence
- Small clinical trial: daily pomegranate juice reduced carotid artery wall thickness after 1 year.
- Improved blood flow in people with CAD.
Typical intake
50–250 mL of pure, no sugar, organic pomegranate juice daily.
Turmeric (curcumin)
A spice from the turmeric root with anti-inflammatory and antioxidant effects.
How it helps the heart
- Reduces inflammation in artery walls, which reduces the risk of artery hardening
- Lowers oxidised LDL, which reduces the risk of artery hardening
- May improve blood flow in the arteries
- Helps maintain artery flexibility
Evidence
- Studies show curcumin reduces CRP (inflammation) and LDL cholesterol levels.
- May improve blood flow and oxygen in people with metabolic syndrome and diabetes.
Typical dose
- 500–1000 mg/day curcumin
- Supplements usually contain black pepper for better curcumin absorption
Meditation and mindfulness
Meditation is a way to achieve a calmer state of mind and mental clarity. Techniques focus on breath, sounds or a mantra to reduce stress and enhance wellbeing.
Meditation and mindfulness
- Reduces the stress hormones, especially cortisol
- Lowers blood pressure and heart rate
- Improve heart rate variability (HRV) — a sign of better cardiac balance
- Help manage anxiety and depression (common in CAD)
Yoga
Combines movement, breathing, and relaxation — shown to:
- Lower blood pressure and LDL (bad) cholesterol
- Improve the function of artery cells walls
- Reduce stress and inflammation markers
Traditional herbal medicines
Always consult your doctor before using herbs as they can interact with heart medications, especially blood thinners and statins
Hawthorn (Crataegus spp.)
Hawthorn has been traditionally used for hundreds of years in Europe to support and strengthen the heart.
Studies do show moderate evidence that hawthorn is beneficial for the heart:
- Improves heart muscle contraction and circulation
- Increases and improves blood flow to the heart
- Has antioxidant and anti-inflammatory properties, to protects against damage to the artery walls and reduces inflammation in the heart
- It is used in Europe for mild heart failure as an extra treatment alongside conventional medications
Hawthorn won’t stop angina and should never be used instead of your heart medicines. It can interact with many heart medicines, so always consult your doctor if you want to take it.
Guggul (Commiphora mukul)
There is limited evidence (in older studies nothing recent) that it may reduce cholesterol.
Ginkgo biloba
Ginkgo biloba is one of the most common herbs used in Europe.
- It is an antioxidant and improves blood flow in the left anterior descending coronary artery
- Helps blood vessels open up to allow better blood flow
- Has anti-inflammatory properties
- Studies show it generally improves blood flow throughout the whole body, which is why it has been used in Europe to improve blood circulation in the legs and hands
Ginkgo biloba won’t dissolve a blood clot, there’s not enough clinical trials to confirm these results and it should never be used instead of your heart medicines. It can interact with many heart medicines, so always consult your doctor if you want to take it.
Red yeast rice
Naturally contains compound monacolin K which is chemically identical to the active ingredient in statins. Studies prove red yeast rice does reduce LDL cholesterol and overall cholesterol. As it’s a food, the amount of monacolin K in red yeast rice varies. There is also concern about it being contaminated by citrinin a mycotoxin that is toxic to human health.
Acupuncture
Acupuncture is considered safe as an addition to your treatment, along with your medications:
- May improve blood flow and reduce stress-related angina
- Some studies show acupuncture reduces chest pain frequency and intensity in stable angina
Self care
Coronary artery disease self care
There are many strategies you can take to help keep yourself healthier.
- Monitor your blood pressure and cholesterol on a regular basis.
- Maintain regular physical activity suited to your condition. Aim for at least 30 minutes of some form of exercise every day.
- Eat balanced, anti-inflammatory meals by eating a Mediterranean type diet, which includes, olive oil, berries, leafy greens, legumes.
- Avoid trans fats and excessive salt. These are usually found in processed foods but don’t add too much salt to your foods.
- Limit alcohol to less than 2 standard drinks a day (men), less than 1 standard drinks a day (women).
- Prioritise sleep by getting 7–9 hours each night.
- Engage in social support networks — positive emotional health correlates with better cardiac outcomes and a healthier heart.
- Manage stress through relaxation techniques or cognitive-behavioural therapy.
References
References
- Arbab-Zadeh A, et al. Diagnostic accuracy of CT angiography for coronary artery disease. J Am Coll Cardiol. 2012;59(19):1914–1923.
- Australian Department of Health, Disability and Ageing. Physical activity and exercise guidelines for all Australians. Accessed 7 November 2025
- Aviram M, Dornfeld L, Rosenblat M, Volkova N, Kaplan M, Coleman R, Hayek T, Presser D, Fuhrman B. Pomegranate juice consumption reduces oxidative stress, atherogenic modifications to LDL, and platelet aggregation: Studies in humans and in atherosclerotic apolipoprotein E-deficient mice. Clinical Nutrition. 2004;23(3):423–433.
- Basu A, Sanchez K, Leyva MJ, Wu M, Betts NM, Aston CE, Lyons TJ. Green tea supplementation affects body weight, lipid profile, and lipid peroxidation in obese subjects with metabolic syndrome. American Journal of Clinical Nutrition. 2011;93(3):550–559.
- Bhatt, Deepak L., Steg, Philippe G., Miller, Michael, Brinton, Eliot A., Jacobson, Terry A., Ketchum, Sherrie B., Doyle, Robert T. Jr., Juliano, Richard A., Jiao, Lixin, Granowitz, Christopher, and Tardif, Jean-Claude. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. New England Journal of Medicine. 2019;380(1):11–22.
- Budoff MJ, et al. Assessment of coronary artery disease by cardiac CT. Circulation. 2016;133(25):2719–2745.
- Cicero AFG, Colletti A. Nutraceuticals and blood pressure control: Results from clinical trials and meta-analyses. High Blood Press Cardiovasc Prev. 2015;22(3):203–213.
- Del Gobbo, Liana C., Imamura, Fumiaki, Wu, Jason H.Y., de Oliveira Otto, Marcia C., Chiuve, Stephanie E., and Mozaffarian, Dariush. Circulating and dietary magnesium and risk of cardiovascular disease: A systematic review and meta-analysis of prospective studies. BMC Medicine. 2013;11:187.
- Estruch R, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279–1290.
- Farkouh ME, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367:2375–2384.
- Fihn SD, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for diagnosis and management of stable ischemic heart disease. Circulation. 2012;126(25):e354–e471.
- Fotino, Andrea D., Thomson, Lindsay, Hagar, John, and Dundas, Nicole. Coenzyme Q10 supplementation and heart failure: A systematic review. American Journal of Clinical Nutrition. 2013;97(2):268–275.
- Gao, Dian, Ning, Ning, Wang, Chunyu, Wang, Yue, Li, Quan, and Zhang, Ming. Fish oil supplementation and risk of coronary heart disease: Meta-analysis of randomized controlled trials. Atherosclerosis. 2013;226(2):328–334.
- Grundy SM, et al. 2018 AHA/ACC guidelines on cholesterol management. J Am Coll Cardiol. 2019;73(24):e285–e350.
- Gulati M, et al. 2021 AHA/ACC Chest Pain Guidelines. Circulation. 2021;144(22):e368–e454.
- Gupta SC, Patchva S, Aggarwal BB. Therapeutic roles of curcumin: Lessons learned from clinical trials. AAPS J. 2013;15(1):195–218.
- Hillis LD, et al. 2011 ACCF/AHA Guideline for coronary artery bypass graft surgery. Circulation. 2011;124(23):e652–e735.
- Houston M. Nutraceuticals, vitamins, antioxidants, and minerals in the prevention and treatment of hypertension. Prog Cardiovasc Dis. 2005;47(6):396–449.
- Kass L, Weekes J, Carpenter L. Effect of magnesium supplementation on blood pressure: A meta-analysis. European Journal of Clinical Nutrition. 2012;66(4):411–418
- Knuuti J, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–477.
- Jayasinghe SR. Meditation and cardiovascular health: An updated review. Complement Ther Clin Pract. 2016;23:9–14.
- Lavretsky H, Irwin MR. Stress and inflammation in coronary heart disease. Neurobiol Dis. 2021;155:105385.
- Li S, Li J, Deng X, et al. Aged garlic extract reduces blood pressure in hypertensives: A systematic review and meta-analysis. Exp Ther Med. 2020;19(2):1472–1480.
- Li L, et al. Effects of meditation on heart rate variability and stress reduction in patients with coronary heart disease: A systematic review. Front Cardiovasc Med. 2022;9:876543.
- Libby P, Buring JE, Badimon L, et al. Atherosclerosis. Nat Rev Dis Primers. 2019;5(1):56.
- Lin P, Yu Y, Wu Y, Zhang X, Zhang R, Zhang Z, Zhang Y. Effects of green tea or green tea extract on nonalcoholic fatty liver disease and cardiovascular risk factors: A meta-analysis. Journal of Translational Internal Medicine. 2020;8(4):180–189.
- Jayasinghe SR. Meditation and cardiovascular health: An updated review. Complementary Therapies in Clinical Practice. 2016;23:9–14.
- Madmani ME, et al. Coenzyme Q10 for heart failure. Cochrane Database Syst Rev. 2014;(6):CD008684.
- Maulik SK, Katiyar CK. Hawthorn (Crataegus oxyacantha) in cardiovascular disorders: A review. Phytother Res. 2010;24(5):659–665.
- Mozaffarian D, Wu JHY. Omega-3 fatty acids and cardiovascular disease: Effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol. 2011;58(20):2047–2067.
- Neumann FJ, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165
- Niering P, Hermsdorf H, Wilke A, Schuler G. Effectiveness of yoga-based cardiac rehabilitation after acute coronary events. European Journal of Preventive Cardiology. 2015;22(8):911–918.
- Ornish D, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280(23):2001–2007.
- Panahi Y, Khalili N, Sahebi E, Namazi,S, Reiner Z, Majeed M, Sahebkar A. Curcuminoids modify lipid profile in type 2 diabetes mellitus: A randomized controlled trial. Complementary Therapies in Medicine. 2017;33:1–5.
- Pang J, Zhang Z, Zheng T, Song W. Green tea consumption and risk of cardiovascular disease: A meta-analysis of prospective cohort studies. American Journal of Clinical Nutrition. 2016;104(6):1679–1692.
- Park E-K, Han K-H. Effects of meditation on heart rate variability and stress reduction in patients with coronary heart disease: A systematic review. Frontiers in Cardiovascular Medicine. 2022;9:876543.
- Patel C, Marmot MG, Terry DJ, Carruthers M, Hunt B, Jenkins D. Trial of relaxation and stress management in chronic stable angina. Lancet. 1975;1(7914):1053–1055.
- Reid K, Fakler P, Stocks NP. Garlic lowers blood pressure in hypertensive individuals, regulates serum cholesterol, and stimulates immunity: A meta-analysis. BMC Cardiovasc Disord. 2008;8:13.
- Reid K, et al. Effect of garlic on blood pressure and cholesterol. Nutr Res Rev. 2016;29(1):55–68.
- Reid K, Fakler P, Stocks, NP. Garlic lowers blood pressure in hypertensive individuals, regulates serum cholesterol, and stimulates immunity: A meta-analysis. BMC Cardiovascular Disorders. 2008;8:13.
- Reinhart K M, Talati R, White CM, Coleman CI. The impact of garlic on lipid parameters: A systematic review and meta-analysis. Annals of Internal Medicine. 2009;150(4):292–300.
- Rizza S, et al. Endothelial function and cardiovascular risk in patients with coronary artery disease: Role of polyphenols. Nutrients. 2020;12(8):2390.
- Rosenfeldt, Fred L., Haas, Stephen J., Krum, Henry, Hadj, Angelica, Ng, Karen, Leong, Jenny Y., Watts, George F., and Uvarov, Oleg. Coenzyme Q10 in the treatment of hypertension: A meta-analysis of the clinical trials. Journal of Human Hypertension. 2007;21(4):297–306.
- Sahebkar A, Serban M-C, Ursoniu S, Banach M. Effect of curcuminoids on oxidative stress: A systematic review and meta-analysis of randomized controlled trials. Clinical Nutrition. 2015;34(6):1101–1108.
- Simental-Mendía, Luis E., Sahebkar, Amir, Rodríguez-Morán, Martha, and Guerrero-Romero, Fernando. Effects of coenzyme Q10 supplementation on lipid profiles: A systematic review and meta-analysis. Current Pharmaceutical Design. 2017;23(10):1470–1475.
- Stone GW, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting in patients with three-vessel or left main coronary artery disease. N Engl J Med. 2016;375:2223–2235.
- Sumner MD., Elliott-Eller M, Weidner D, Daubenmier JJ, Chew MH, Marlin R, Raisin CJ, Ornish D. Effects of pomegranate juice supplementation on myocardial perfusion in patients with coronary heart disease. American Journal of Cardiology. 2005;96(6):810–814.
- Virdis A, et al. Magnesium and cardiovascular risk. Nutrients. 2021;13(2):626.
- World Health Organization. Alcohol. Accessed 7 November 2025
- World Health Organization. Cardiovascular Diseases (CVDs). WHO; 2023.
- Yusuf S, et al. Global burden of cardiovascular diseases. Circulation. 2020;142(23):2068–2090.
- Zhang X, Pan Y, Huang Z, Cai W, Li Y, Wang C. Pomegranate juice supplementation improves lipid profiles and oxidative stress in patients with coronary heart disease: A randomized clinical trial. Atherosclerosis. 2020;313:11–17.
- Zhao L, Li D, Zheng H, Chang X, Cui J, Wang R, Wang W. Acupuncture for angina pectoris: A randomized controlled trial and systematic review. European Journal of Preventive Cardiology. 2012;19(1):24–31..
- Zhao XY, Zhang Y, Wang L, Guo J, Sun Y. Effects of red yeast rice on lipid profiles in patients with hyperlipidemia: A meta-analysis. Annals of Nutrition and Metabolism. 2015;66(2–3):210–218.
- Zhou, Shanshan, Zhao, Ying, Li, Yu, Ma, Hong, Zhang, Li, and Wang, Zhihong. Clinical effects of combined coenzyme Q10 and selenium therapy in patients with ischemic heart disease. Nutrition Research. 2016;36(1):82–88.
Last reviewed and updated: 10 November 2025